Knee arthritis
The knee joint is formed by the upper end of the tibia (shinbone), the lower end of the femur (thighbone) and the patella (kneecap). In the healthy knee, the surfaces of these three bones are covered by articular cartilage which cushions the bones and allows for near-frictionless, pain-free movement. Knee function is further optimised by two cushion-like wedges of fibrocartilage, the medial and lateral meniscus. The knee joint is also surrounded by a thin lining called the synovial membrane. This membrane releases synovial fluid that lubricates the cartilage and reduces friction.
The most common types of arthritis are osteoarthritis and rheumatoid arthritis, but there are several other forms. Osteoarthritis, in particular, is a degenerative, “wear-and-tear” type of arthritis that occurs most often in people 50 years of age and older, but may occasionally occur in younger people too. In osteoarthritis, there is gradual wear of the cartilage that leads to pain, stiffness, instability and a change in limb alignment.
Treatments for knee arthritis
Kostas will thoroughly assess your condition and individual requirements and discuss the appropriate treatment options. These may be surgical or non-surgical.
Non-surgical treatments for knee arthritis
Activity modification, pain relief medication, knee injections, off-loading the lower limb using a walking aid, bracing, physiotherapy and weight loss are the main non-surgical options for the treatment of symptomatic knee arthritis. They can be utilised in isolation or combined and can be effective in addressing the symptoms, but will not alter the actual condition.
Knee replacement surgery
If the non-operative management has failed to address the symptoms, surgery should be considered. Knee replacement surgery is the gold-standard surgical option and involves the removal of the damaged parts of the knee joint, which are replaced by prostheses (implants).
The choice between total and partial knee replacement surgery depends on the patient’s symptoms and radiographic findings. Kostas will thoroughly assess each individual case and will recommend the type of procedure that is most likely to address the symptoms and provide a reliable long-term solution.
Knee replacement surgery is very successful in addressing knee pain and stiffness. All the units that Kostas works with have well-established protocols that can deliver safe perioperative care. Kostas will explain all the benefits and risks associated with this treatment and will answer any relevant questions well in advance of the procedure itself. After the surgery, most patients will stay in hospital for one to three nights and will then continue their rehabilitation outside the hospital for 6 to 8 weeks.
Knee arthroscopy
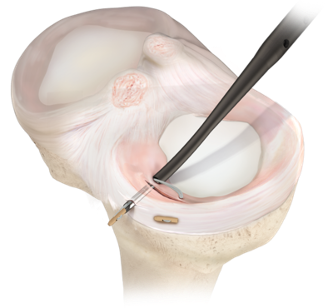
Knee arthroscopy is a surgical technique that uses a minimally invasive, keyhole, approach to diagnose and treat problems in the knee joint. A special camera, called an arthroscope, allows the surgeon to reliably inspect the knee joint and, with the use of specialist instruments, perform a number of different treatments.
Some of the commonest such treatments address tears of the meniscus (meniscal repair or partial meniscectomy) or injuries of the cartilage (microfracture or chondroplasty). Knee arthroscopy can also be employed to provide access during ligament reconstructions, such as for the anterior cruciate ligament, or to help remove a loose body (usually a piece of cartilage from a previous injury).
The right candidate for knee arthroscopy is a patient who is symptomatic with a condition that can be treated arthroscopically and has tried an appropriate course of non-operative management. Before discussing the option of knee arthroscopy, Kostas will have comprehensively assessed the presenting condition and will almost certainly have acquired specialist investigations, such as an MRI scan. Alternatives to surgery, benefits and risks of the surgical treatment, and the specific details of the planned intervention will be clarified before embarking on the surgical management of the condition.
Recovery following knee arthroscopy
The vast majority of treatments using knee arthroscopy can be undertaken as a “day-case” and the patient can expect to be able to mobilise, possibly with crutches, immediately after the procedure. On some occasions, there may be a requirement to “off-load” the operated limb or use a knee brace, such as in cases of meniscal repair or microfracture. The vast majority of patients should expect to return to their daily activities within two to six weeks, but on occasions the recovery may be lengthier, such as in anterior cruciate ligament reconstruction, when six to nine months may be necessary before the patient can return to sports.
Meniscus and meniscal tears
The meniscus is a fibrocartilaginous structure in the knee joint with a complex function. In simple terms, it can be imagined as a “c-shaped” cushion that helps protect the articular cartilage, which in itself is the lining of the bones that allows them to glide smoothly during motion. There are two menisci in each knee, the medial meniscus and the lateral meniscus, either of which can sustain an injury (meniscal tear). These injuries are frequently seen following sports injuries, but can also occur as a result of a degenerative process.
Some meniscal tears can be treated with an initial period of rest and then physiotherapy, the latter with the aim of achieving better conditioning of the muscles of the thigh. However, there are occasions when surgical treatment should be considered, such as when the patient experiences mechanical symptoms that have not improved with the non-surgical treatment. When surgery is considered, Kostas will explain the rationale, the available surgical options the risks and benefits. Whenever possible, repair of the torn meniscus will be pursued, in order to prevent progressive wear of the articular cartilage which results to degenerative arthritis.
Meniscal repair vs partial meniscectomy
Meniscal repair can be performed through knee arthroscopy using a number of specialist techniques and instruments. The aim is to preserve the meniscus and help prevent the onset of degenerative changes in the knee joint. When meniscal repair is not possible, Kostas will perform partial meniscectomy, ie trimming off the part of the meniscus that is causing the symptoms, preserving as much meniscal tissue as possible in the process. The recovery following these treatments differs and Kostas will comprehensively explain the protocols he uses for each.
Anterior Cruciate Ligament (ACL) injury
The ACL is part of a complex set of ligaments in the knee joint. It prevents the tibia from moving too far forward on the femur and keeps the knee from twisting excessively. Anterior cruciate ligament ruptures are relatively common and can affect athletes of all levels, particularly in sports like football and skiing. They often occur during a sudden twisting injury of the knee, such as when a person stops quickly, plants his/her leg and changes direction. ACL injuries can often be accompanied by injuries to other tissues in the knee, including the menisci, the cartilage or other ligaments.
Common symptoms of a torn ACL include a popping sound at the time of the injury, pain, swelling and knee instability. In the short- to mid-term, patients may experience inability to jump and land, accelerate and change direction, or pivot on the knee. A torn ACL can usually be diagnosed through a careful history and clinical examination. MRI scanning is very helpful in order to confirm the ACL rupture and assess for other injuries of the knee and surrounding tissues.
ACL treatment options
Once torn, the ACL cannot regrow or heal on its own. Based on your individual circumstances, Kostas will make a careful assessment and recommend treatment. This may include measures to alleviate the acute symptoms, physiotherapy with an ACL-specific rehabilitation protocol or, if needed, ACL reconstruction surgery. The choice to have surgery is based on the patient’s lifestyle, response to rehabilitation and individual expectations.
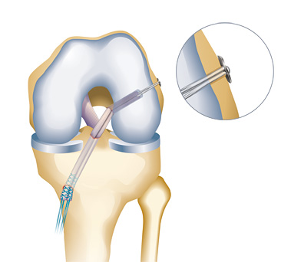
In terms of surgery, ACL reconstruction involves replacing the ligament with a tendon graft. The graft usually comes from the injured person’s hamstring tendons, but patellar tendon and quadriceps tendon can also be used. An allograft (human donor tissue) may also be considered in some cases. Kostas will thoroughly explain the rationale for the choice of graft and the steps of the procedure, as well as the benefits and risks involved.
Patients who undergo ACL reconstruction surgery can move their knee immediately after the procedure and can return home the same day. The procedure can be undertaken under regional or general anaesthetic. A review by a physiotherapist will be undertaken on the day of the procedure and the rehabilitation programme will begin within the following week. People are expected to be able to run in three to four months and return to their sports in eight to ten months. Kostas will be reviewing your progress during that time.